All About Aspiration
“It went down the wrong pipe,” “I swallowed it the wrong way,” “I think I choked, but I’m fine now.” These are common sayings we’ve all likely said or heard at some point throughout our lives. That sensation of food going down the wrong pipe is called aspiration. Have you heard of it? Aspiration is when food, saliva, or stomach acid enters our airway accidentally. Typically speaking, when aspiration occurs, we cough until we feel better, and then carry on with our day. Not surprisingly, aspiration is relatively common, and by itself does not cause pneumonia. But why, and how, does aspiration pneumonia then occur? Let’s shed some light on aspiration, and its link to pneumonia.
What happens if I aspirate?
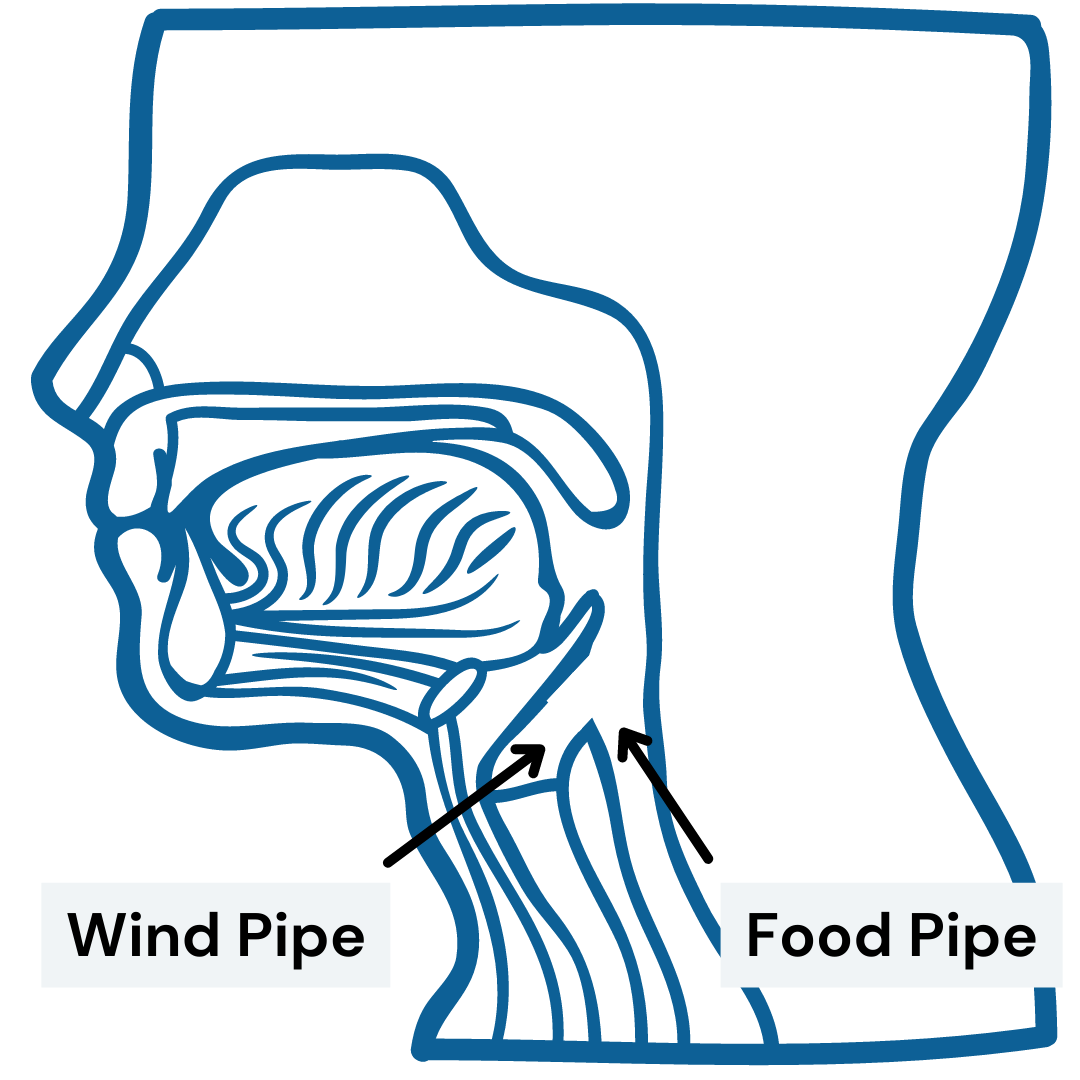
Swallowing is a complicated process that we all do with minimal conscious awareness. These sets of motor movements include preparing food or liquid, initiating the swallow, and then sending the swallowed item(s) to the stomach. We do this without thought, all while avoiding the airway (which is honestly way too close to the entrance to the stomach). It seems like a lot of work for something we barely pay attention to, but our bodies are amazing, right?
In healthy adults, aspiration is typically not a problem as long as it does not occur frequently. We all aspirate at times. It's completely normal, and aspiration alone does not cause pneumonia or infection. But when individuals have trouble chewing or swallowing, especially those with underlying conditions (e.g., neurodegenerative diseases, compromised immune systems, etc.), they become at risk for increased aspiration, potentially leading to serious health complications or aspiration pneumonia.
What exactly is aspiration pneumonia?
If you are having trouble swallowing, your doctor may have told you that you are aspirating and are at risk for aspiration pneumonia. I'm sure it sounds frightening to hear that, but the truth is that aspiration pneumonia is not as cut and dry as we may think. Aspiration pneumonia is a vague diagnosis that includes at least 13 different conditions, including community-acquired pneumonia, hospital-associated pneumonia, ventilator-associated pneumonia, and so on. Remember, aspiration is when ANY substance enters the lungs, including a virus or bacteria.
For these reasons, aspiration pneumonia does not just occur as an independent disease on its own. Instead, it is a secondary disease that depends upon the presence of a serious illness resulting from a disease or medical condition. Aspiration can be serious and can cause sickness, but there are many factors to consider when thinking about the likelihood of developing aspiration pneumonia. Aspirating does not immediately lead to aspiration pneumonia.
Risk factors of aspiration pneumonia
General Health
Individuals in good health easily fend off the potential negative effects of mild-to-moderate aspiration. Individuals with poor health have an increased risk of a negative event occurring from aspiration.
Individuals who are frail or deconditioned are likely to have a negative event occurring from aspiration due to reduced functional abilities, and poor coping strategies, causing further decompensation.
Cognition
Reduced cognitive function impacts swallow safety, whether acute or chronic.
For individuals with chronic cognitive decline, a referral can be made to a speech-language pathologist for strategies, diet modifications, and education to reduce the incidence of aspiration and avoid adverse events.
Medical conditions
Overall medical status can impact one's ability to cope with aspiration
For individuals who are relatively healthy prior to an acute event (such as a stroke or brain injury), the impact of aspiration is less likely to cause a negative/adverse outcome.
For individuals with chronic disease, there is an increased likelihood of a negative outcome occurring from aspiration
Specifically, certain medical conditions place individuals at a greater risk of aspiration pneumonia or adverse events When multiple diseases co-occur, the risk is amplified. These medical conditions include:
Respiratory or pulmonary disease
Gastrointestinal disease
Immunocompromised status
Oral Health
Good oral health helps reduce the growth and colonization of bacteria in the airway tracts. If oral contents are aspirated with a high bacterial load, this can cause harmful damage to the respiratory system. So make sure you brush your teeth and go to the dentist regularly!
Oral bacteria should be kept at a minimum through the use of oral care, which includes adequate cleaning of the surfaces in the oral cavity (tongue, teeth, cheek, palate). By not cleaning thoroughly and consistently, there is potential for increased bacterial growth.
Materials
Not all aspirated materials have the same effect! Materials that enter the airway can vary by the amount, chemical makeup, and density. Large volumes and density, and highly acidic materials are more likely to lead to infection. High acidity can alter and damage fragile lung tissue, thus causing greater harm if aspirated.
Aspiration of food vs. liquids is a greater risk for adverse events, as well as aspiration of thickened liquids vs. thin liquids. This is because aspiration of solids requires greater strength and respiratory responses for successful removal. Thickened liquids are also harder to clear from the lungs.
Dependency
Individuals who are dependent on others for oral care, nutrition, and hydration are at increased risk for aspiration. This is due to the varying feeding styles, speeds, and volumes. For individuals with dependency, a referral to a speech-language pathologist can assist with training for safe swallow strategies and education on swallowing modifications and physiology.
Individuals who have mobility issues and are dependent on others to move around are more likely to aspirate as frequent mobility has a positive impact our our pulmonary system.
Tubes
Individuals that have tubes, such as a trach tube or feeding tube, may harbor bacteria that is transferred to the lungs during aspiration or microaspiration events, increasing the risk of negative outcomes.
Mechanical ventilation
Being placed on mechanical ventilation (assisted breathing) can damage even healthy lungs, resulting in increased lung swelling. This may result in ventilator-induced lung damage and aspiration.
What you need to remember
Aspiration is a normal occurrence and only becomes a problem if it happens frequently and in the presence of other health and lifestyle factors. Some simple things you can do to make sure you reduce your risk factors include brushing your teeth, tongue, and gums after every meal and keeping your respiratory health strong by moving your body. If you or your loved one are having difficulty swallowing and are concerned about aspiration pneumonia, a skilled speech-language pathologist can help rehabilitate the swallow, provide compensatory strategies to improve safety and educate about changes that are occurring. The sooner you act, the better the outcomes you will see. So if this is of any concern, please call the SLPs at Neuro Speech Solutions for a consultation and personalized treatment plan.
ABOUT THE AUTHOR
Annie Rabe, MS, CCC-SLP
Annie is a speech-language pathologist with experience in many settings. From acute care to home care, she has helped her patients get back to the activities they love doing. She believes that developing a strong relationship with her clients and their family is the foundation for successful therapy.




Are you having trouble swallowing and your doctor warned you about aspiration? Maybe they even told you that you are at risk for aspiration pneumonia! It’s time to breakdown what this actually means and how likely you are to acquire it. Read on for some education. 6 Min Read